A malignant tumor is a bustling metropolis populated by many different kinds of cancer cells. This cellular diversity, however, is what makes cancer so difficult to treat, as each type of cell in a tumor responds differently – and sometimes not at all – to cancer therapies. This is especially true for lung cancer, which often responds to an initial course of treatment, only to remerge after becoming drug-resistant, making it the deadliest form of cancer worldwide.
A better understanding of the diversity that exists within a lung tumor would likely lead to more effective treatments. Today, clinicians generally rely on tests that generate genetic profiles of biopsied tumors in bulk rather than one cell at a time. Unfortunately, this usually fails to capture the full extent of cellular diversity within tumors and ends up obscuring clinically significant information. This has led scientists to search for ways to assemble a census of the many types of cells that comprise a malignant tumor. Even better would be a more complete picture of how these cell populations evolve during the course of treatment. However, figuring out exactly how to conduct this survey has proven to be a major technical barrier for scientists.
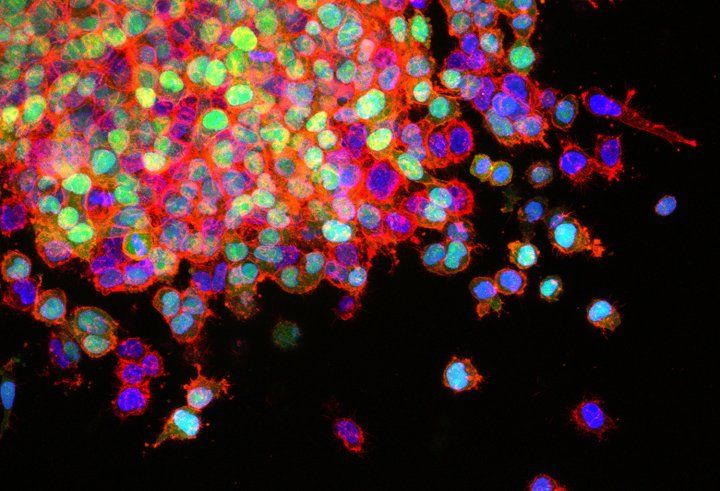
But this hurdle, once thought to be nearly insurmountable, was recently cleared by a research team led by UC San Francisco and Chan Zuckerberg Biohub scientists. The researchers figured out how to assemble genetic profiles of individual lung cancer cells obtained from patients at different times during the course of their treatment. In doing so, they revealed a vast cornucopia of cellular diversity in both lung tumors and the tissue surrounding the tumor as they evolved during the course of treatment – clinically significant information that had previously eluded scientists. The findings are detailed in a paper published Aug. 20 in the journal Cell.
“This study is among the first of its kind,” said Trever Bivona, MD, PhD, professor of medicine and senior author of the study. “We observed features of lung cancer cells and the tumor microenvironment that no one had seen before. This gave us a window into the evolution of individual cells within the tumor’s ecosystem.”

Starting with 49 biopsies obtained from 30 lung cancer patients, the researchers used single-cell sequencing to map the landscape of gene activity in over 23,000 individual lung cancer cells at three time points: before treatment, after the tumors stabilized or went into remission during treatment, and after the cancer, despite continuous treatment, had fully re-grown and become treatment resistant.
These single-cell profiles revealed the presence of tumor cells that harbored cancer-driving genetic mutations distinct from those that were identified by the various clinical tests that the patients received during the course of their treatment. Though these mutations were present in only a fraction of cells in each tumor, they had a significant effect on patient outcomes. Patients whose tumors carried two or more of these mutations had significantly lower overall survival rates than patients with fewer than two.
The researchers also found that when lung tumors stabilized or went into remission in response to treatment, some malignant cells were able to cling to life by switching on genes associated with injury repair and survival that are normally only active in healthy lung cells. When these genes are active, the cancer cells enter a repair and survival state that, according to Bivona, “puts the cells into hibernation mode so that the cell death machinery doesn’t get activated.”
But these survival genes have an Achilles’ heel. They rely on what’s known as the Wnt/beta-catenin signaling pathway, which can be targeted with existing drugs. In fact, laboratory tests demonstrated that when administered at the appropriate time, drugs targeting the Wnt/beta-catenin pathway, combined with a common lung cancer therapy, reduced the number of cancer cells that survived.
“Our results suggest that we could target specific cell states in lung tumors and improve patient survival by constraining tumor evolution and preventing drug resistance and tumor survival and re-growth,” Bivona said.
The study also provides key insights into how the cells and tissue that surround a lung malignancy – the tumor microenvironment – create conditions that prevent the immune system from taking up arms against the tumor.
Single-cell profiling revealed that the tumor microenvironment was hostile to immune activity both before treatment and after a tumor had evolved drug resistance. However, during treatment, when the cancer is in the “hibernation mode” revealed in the study, the researchers found that immune cells were able to infiltrate the tumor microenvironment and appeared to be switched on, suggesting there may be a limited window of opportunity during which conventional cancer therapies can be combined with immunotherapies – a class of cancer treatments that has proven effective against some cancers, but has largely failed against the types of lung tumors profiled in this study – to produce better overall survival rates.
“Putting tumor heterogeneity front and center would better equip clinicians with information that allows for a high-resolution window into the evolution of tumors during therapy, and help us use such a roadmap to intervene more proactively to better control tumors and help patients,” said Bivona. “The single-cell analysis that we proved is feasible in real-life clinical tumors may help usher in a new era in the clinical management of tumors during therapy by strengthening our molecular diagnostic toolkit.”
Authors: Additional authors include Caroline E. McCoach, Franziska Haderk, D. Lucas Kerr, Elizabeth A. Yu, Philippe Gui, Tasha Lea, Wei Wu, Anatoly Urisman, Kirk Jones, Pallav K. Kolli, Eric Seeley, Yaron Gesthalter, Sourav Bandyopadhyay, Khyati Shah, Lauren Cech, Nicholas J. Thomas, Anshal Gupta, Mayra Gonzalez, Hien Do, Lisa Tan, Bianca Bacaltos, Matthew Gubens, Thierry Jahan, Johannes R. Kratz, David Jablons, Jonathan Weissman, and Collin M. Blakely of UCSF; Ashley Maynard, Lincoln Harris, Weilun Tan, Alexander Zee, Michelle Tan, Rene Sit, Daniel D. Le, Kevin A. Yamauchi, Rafael Gomez-Sjoberg, Norma Neff, and Spyros Darmanis of Chan Zuckerberg Biohub; Julia K. Rotow of Dana-Farber Cancer Institute; and Erin L. Schenk, David M. Naeger and Robert C. Doebele of the University of Colorado.
Funding: This research was supported by NIH awards U54CA224081, R01CA204302, R01CA211052, R01CA231300, R01CA169338, U01CA217882, R01CA227807, T32 HL007185, and K12 CA086913; the Van Auken Foundation; Novartis Pharmaceuticals; Pfizer; the University of California Cancer League; AstraZeneca; The Damon Runyon Cancer Research Foundation award P0528804; Doris Duke Charitable Foundation award P2018110; V Foundation award P0530519l; and the Mildred Scheel postdoctoral fellowship from the German Cancer Aid.
Disclosures: See manuscript for a full list of disclosures.
"time" - Google News
September 04, 2020 at 04:07AM
https://ift.tt/2EOa6mh
Mapping Genetic Diversity of Lung Tumors Over Time May Lead to More Effective Therapies - UCSF News Services
"time" - Google News
https://ift.tt/3f5iuuC
Shoes Man Tutorial
Pos News Update
Meme Update
Korean Entertainment News
Japan News Update
Bagikan Berita Ini














0 Response to "Mapping Genetic Diversity of Lung Tumors Over Time May Lead to More Effective Therapies - UCSF News Services"
Post a Comment